Corneal Cross-Linking (CXL)
Cross-linking is a method that appeared in many country relatively recently, but it has been used all over the world since 2004. Corneal collagen crosslinking is also known as crosslinking method, CXL method, UV-x-linking, UVA method, C3-R. Its Essence consists in photopolymerization of stromal fibers, which occurs under the combined action of a photosensitizing substance (Riboflavin or vitamin B2) and ultraviolet.
During recent years, there has been a noticeable expansion of cross-linking. For example, it is successfully used to prevent the progression of secondary keratoconus (arising after LASIK iatrogenic keratoectasia), pellucid marginal dystrophy, keratomalacia of various origins. There are preliminary encouraging data on the successful use of cross-linking for the treatment of bullous keratopathy, keratitis and corneal ulcers.
The history of the method
The beginning studies of the photobiology of the cornea refers to 1990. Then a group of researchers has been seeking biological adhesives, activated with heat or light, which reinforce the resistance of the collagen of the cornea (Khaderm, T. Tuong, T. J. Emest, 1994). A bonding effect was found to occur in the elimination of oxygen radicals, the release of which caused the formation of bonds of disparate collagen fibrils.
In the opinion of the researchers, the increased resistance of the tissues of the cornea stop the progression of keratoconus and, therefore, postpones or allows you is to avoid transplantation of the cornea patients.
Pioneers of crosslinking were: Professor T. Zeiler, E. Sporl, Wollensak. The idea of this method arose from Professor Zeiler during a visit to the dentist, after he was put photopolymer seal. In 1994, he led a team of researchers, and work began. The first experiments were carried out on animals, and then – on the donor (cadaver) cornea. After that, the first treatment of patients with keratoconus and other keratoectasia was carried out.
The mechanism of corneal cross-linking
- Combined effect of Riboflavin and UltraViolet;
- Release of oxygen radicals;
- The occurrence of coupling between the carbon base – collagen crosslinking.
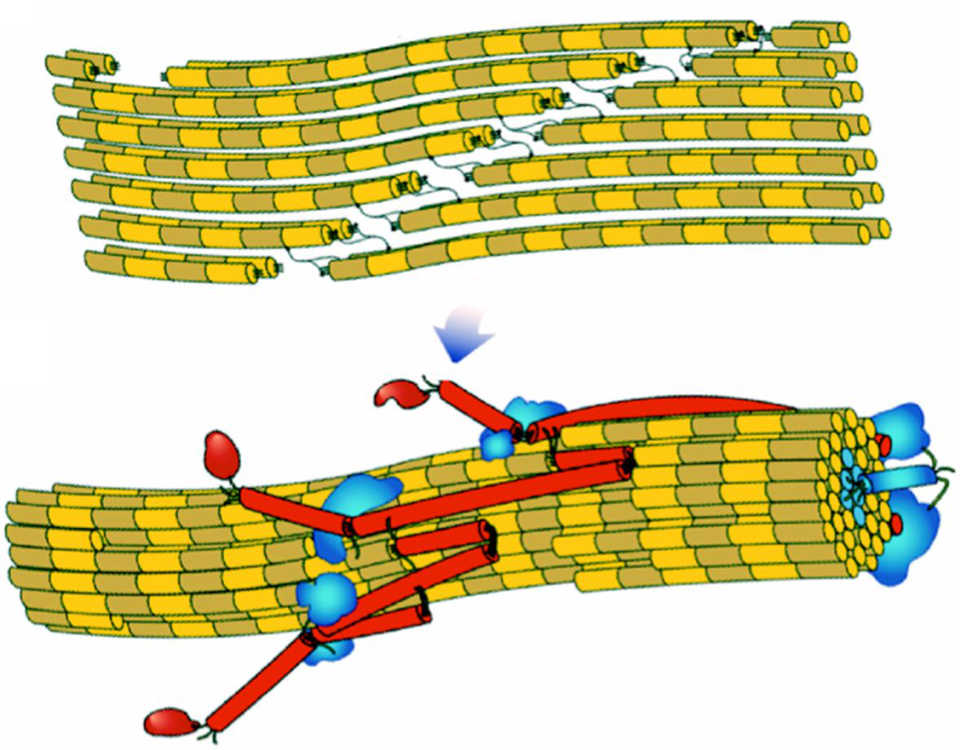
Photopolymerization increases the strength of corneal collagen (rigidity) and increases its resistance to keratoectasia. Between collagen fibrils appear new cross-linking, and it increases the strength of the entire cornea.
Indications for CXL
Due to the relative youth of the method and the development of scientific thought, the scope of cross-linking is growing from year to year, its effectiveness is revealed with an increasing number of diseases. Therefore, we present the testimony formulated by Professor Seiler himself at the cross-linking courses during the international Congress in Berlin in September 2008. The crosslinking is recommended in cases:
- keratoconus (KC);
- pellucid marginal dystrophy (PMD);
- iatrogenic keratoectasia due to LASIK surgery;
- кkeratomalacia-melting of the cornea (cornea melting), which occurs, as a rule, due to autoimmune processes;
- bullous keratopathy

Contraindications
- the thickness of the cornea is less than 400 microns in at least one dimension (although it should be noted that this threshold has ceased to be so categorical after the appearance of solutions causing edema of the cornea);
- low visual acuity with correction in the case of keratoconus, even in the presence of adequate thickness of the cornea;
- patient's age is less than 12 years (not olways);
- corneal scars on huge area;
- allergic conjunctivitis.
Procedure
Manipulations are carried out under local anesthesia (drops of Alkaine). Currently, two main techniques are used - traditional and transepithelial corneal crosslinking.
Conventional cross-linking
The operation is divided into 2 stages.
Stage 1: anesthesia Is performed, the spatula deepithelization of the cornea is carried out, and then the solution of Riboflavin is instilled for 25-30 minutes. After that, the doctor using a slit lamp assesses the degree of impregnation of the cornea drug. If the impregnation is sufficient, proceed to stage 2, if not-continue to instill until the desired result.
Stage 2 is to use a beam of ultraviolet light that interacts with Riboflavin, causing crosslinking of corneal collagen. This process also lasts about 30 minutes.
At the end of the operation, the antibiotic and anti-inflammatory drug are instilled, after which the patient is put on a soft therapeutic contact lens.
Transepithelial corneal collagen cross-linking (TE-CXL)
When using this technology, the removal of the top layer of the cornea is not required. He razryhlenija and becomes permeable to Riboflavin using spetsialnogo of the drug (tetracaine). In this regard, the patient is much less pronounced discomfort after surgery, much shorter rehabilitation period and less risk of various complications.

Possible cross-linking complications
For a long time, the complications of cross-linking were not mentioned in the professional literature. For the first time reports covering this topic appeared at the last ESCRS Congress. In our practice of cross-linking we also meet with typical complications:
- Varying degrees of severity of turbidity of the cornea. The quality of vision is usually not affected, but can be quite pronounced. Most often resorption occurs within 1-6 months, although it happens that this process takes up to 2 years.
- Eye irritation (1-2 weeks after surgery).
- Delay in re-epithelialization.
- Deterioration of the original visual acuity and its gradual recovery. This complication occurs rarely, vision is restored within 1-12 months.
- Melting of the cornea.
- Reactivation of herpetic infection, development of herpetic keratitis.
It should be noted that with all these complications, as a rule, it is possible to cope, and the use of transepithelial technology minimizes risks.
Video of the surgery of crosslinking in keratoconus
Results after crosslinking
It should be understood that since cross-linking has been practiced since 2004, full information about all the results, as well as about all the complications, is still unknown. But some conclusions are possible to do already now, in particular with regard to the application of crosslinking in keratoconus. With this method, it is possible to stop the development of the disease – this is the main result. There are no data on the progression of keratoconus after cross-linking surgery to date.
After surgery, 25% of patients have improved visual acuity by 1-2 lines-this is a consequence of the flattening of the cornea. Since the main task facing cross-linking with keratoconus is to stop the development of the pathological process, the effect of improving visual acuity is a pleasant "bonus". It is not yet clear why some patients have it, while others do not, so it is impossible to plan. In addition to this effect, 30% of patients improve the fit of hard contact lenses, which is made possible due to the same flattening of the cornea.
The price of cross-linking (CXL)
The cost of surgery in our specialized ophthalmological center is 34 000 rubles (530$) with the traditional method. With the technology of transepithelial cross-linking, the drug is additionally paid (about 5,000 rubles - 80$).
Feedback from patients after surgery
Below in the comments you can find other reviews of people who have already passed the procedure of corneal cross-linking or leave your own opinion.




Then discomfort during the day, the lenses of course help, but not at all.
Well, then it grows rapidly...
Some docs say the other segment from the CXL. Thank you in advance.
It all depends on the specific situation, there are various options for the treatment of keratoconus.
In the initial stages, usually, first held collagen crosslinking, then-implanted corneal segments (in the absence of effect).
In the developed stages of the disease, a simultaneous combination of methods is possible. It all depends on the specialist who leads you: what strategy he holds.
In any case, it is necessary to use both methods.
Explain this improvement or? and still a cloud over the eye. When will the turbidity pass?
Reduced vision in the early postoperative period after crosslinking is a normal phenomenon, because the complete epithelization of the cornea and the cessation of inflammatory processes takes 1-2 weeks.
In some cases, low visual acuity may remain longer (if there are so-called" early stromal opacities"), but after 3 months after crosslinking visual acuity increases or returns to the preoperative level.
Reducing the thickness of the cornea after the procedure of crosslinking with Riboflavin is quite normal. This is due to the so-called "tightening effect" (or "compaction") resulting from the operation + the corneal oedema, which make the cornea more thick, is decreased.
Despite the decrease in thickness, the biomechanical properties improve and the progression of keratoconus slows down.
Thanks
Indeed, after the operation of crosslinking (especially the "traditional" method - with the removal of the epithelium), after the procedure, it is necessary for some time (up to a week) to instill antibacterial drops, which when ingested into the bloodstream (including being absorbed in the lacrimal tract) can be released with milk when feeding.
To avoid harm to the child, you can reduce absorption by closing the lacrimal points (as recommended) to refuse during rehabilitation from breastfeeding (decant, use the mixture), as well as to use the method of transepithelial corneal crosslinking (without removing the epithelium), the rehabilitation period is much less, because it is not necessary to remove the corneal epithelium.
The question about improving vision... Will recover it's vision and for what period of time ?. So far all as it was, the image is blurred bifurcates
Thanks .
You should understand that corneal cross-linking is performed not to improve vision (though such cases are), and for the strengthening of the cornea (the prevention of the progression of keratoconus).
To improve visual function, we recommend implantation of corneal ring segments (ICRS) and do it better before cross-linking.
Scleral lenses is not a treatment, it is only a way of vision correction in keratoconus.
We recommend our patients to first to implant intrastromal corneal segments (ICRS) - in the "soft cornea", then - to do cross-linking (for its "strengthening"). But if the order of crosslinking and ICRS implantation is the opposite-there are no difficulties.
Three days ago I had a crosslinking on the left eye (keratoconus 3 St), photophobia is completely gone, the eye is wide open, no pain or discomfort is not present, but began to worry because the eye I see how to be through the muddy glass. Please tell me when it will gone?
If complaints do not pass within 5-7 days, then this is an occasion to appeal to an ophthalmologist, because it is necessary to exclude the development of possible inflammation.
Your authoritative opinion is required.
Two different doctors offer different sequence of alternation and intervals of procedures: Crosslinking and ring setting, both of which justify their position, but the rationale does not connect logically.
In what sequence in your opinion it is correct to work and with what interval?
CXL is offered to do on both eyes, ICRS is on one. I'm 33. The examination showed astigmatism and acuity-2 in the right eye and on it keratoconus 2 stage rolling in 3. The second eye keratoconus 1 stage and visual acuity -1.
Installation of ICRS is better to carry out with femtolaser support and with the use of author's nomograms (as we do in our clinic) - this gives a much better result in visual acuity than "manual installation without computer calculations" - which is offered to patients in most clinics.
Can you do a crosslinking on my eyes?
If you just go to the gym, you can visit it in 2-3 days after the procedure (when the corneal epithelialization is finished) and the eyes will be comfortable.
it is not clear what your question is, but comment on:
These complaints may be in the first few weeks after the corneal cross-linking procedure, but after 3 months everything should be normal.
As for the "points" - it is not clear where they are located - on the cornea, in float in the vitreous or other localization... In General, if your doctor finds it difficult to interpret the situation - we will be happy to answer all your questions and give recommendations after a intramural examination. Call us!
It is not clear when you started itching - if immediately after the procedure of cross- inking - it may be an allergic reaction - more often on drugs that are prescribed after surgery.
If the eye is scratched after some time, it may not be associated with cross-linking of the cornea, but be a separate symptom for the same Allergy, demodicosis, conjunctivitis, meibomitis, etc.
The rehabilitation period after the corneal cross-linking procedure takes up to 1 month (during this period it is necessary to instill drops).
As for the improvement of vision - it begins to get better, almost from the first day and finally stabilized, usually within a month.