Penetrating keratoplasty (corneal transplantation or PKP)
Keratoplasty - a surgery for corneal transplantation in keratoconus requires approximately 10-20% of patients. The essence of this operation is to remove the keratoconus-affected part of the cornea and replace it with a donor cornea. The percentage of success of keratoplasty and the patient are gaining good vision is about 90%, which is quite high.
Recovery of vision is usually not immediately after surgery. Sometimes it takes several weeks, and in some cases the process takes up to 12 months.
It is also necessary to know that the survival rate of the transplanted cornea is 74% after 5 years after surgery, 64% after 10 years, 27% after 20 years, and after 30 years – only 2%. Surgery, in which only a small part of the cornea (partial keratoplasty) is removed, reduces the risk of graft rejection. High qualification of surgeons performing keratoplasty provides good results of operations.
Indications for penetrating keratoplasty (PKP)
- Optical keratoplasty is performed to improve visual acuity in pseudophakic bullous keratopathy, keratoconus, dystrophy, degeneration, cicatricial lesions.
- Plastic keratoplasty can be used when it is necessary to restore or maintain the integrity of the cornea with severe structural changes, for example, in the case of Descemetocele or thinning of the stroma.
- Therapeutic keratoplasty is used in the absence of the effect of treatment to replace the infected tissue of the cornea.
- Cosmetic keratoplasty is rarely used to correct the appearance of the eye.
IMPORTANT! Penetrating keratoplasty (PKP) in keratoconus and other eye diseases is a difficult, expensive operation with many complications. However, most eye elinics in Russia and in the World do not offer their patients alternatives: Deep Anterior Lamellar Keratoplasty (DALK) and Posterior Lamellar Keratoplasty options (DLEK, DSEK, DMEK). In our international ophthalmologic center there are necessary transplants, technologies and specialists to offer the patient that option which will be effective in his case and with guarantee will improve sight!
Corneal graft for PKP
Previously, there have been quite large difficulties with corneal transplantation, because the implementation of tissue sampling from the donor was carried out no later than 24 hours after death. For these purposes, do not use the cornea of infants, because they have a great flexibility, which causes the formation of high astigmatism. The cornea of the elderly (over 70 years) have a low density of endothelial cells, so they are also considered unsuitable. Before the operation, the donor tissue is examined, at least, with the help of a slit lamp, and best of all - with the use of biomicroscopy.
It are some contraindication to use the cornea in the following cases:
- Unknown cause of death.
- If you have the donor for infectious diseases of the CNS (system sklerosiruuschem of panencephalitis, progressive multifocal leukoencephalopathy).
- If the donor has some systemic infections (AIDS, Viral Hepatitis, Syphilis, Septicemia).
- If the donor has leukemia and disseminated lymphoma.
- If the donor has eye diseases (malignancies, inflammation in the active stage) and after surgery on the eyes.
Currently, most clinics use "corneal Biotransplant" - a specially treated donor cornea, which can be stored for a long time, which allows ophthalmological centers engaged in end-to-end keratoplasty to have the necessary stock of material.
Prognosis of corneal transplant surgery
Some factors need to be considered before keratoplasty as they may worsen the prognosis of the surgery. These include:
- Anomalies of the eyelids (blepharitis, entropion, ectropion, trichiasis). It must be corrected before keratoplasty.
- Inflammation of the conjunctiva (progressive or recurrent), such as ocular scar pemphigoid, atrophic conjunctivitis.
- Tear film dysfunction.
- Pronounced vascularization of the stroma or thinning of the intended bed.
- Uveitis.
- Frontal sinehias.
- Lack of sensitivity of the cornea or corneal inflammation.
- Uncompensated glaucoma.
The most favorable for keratoplasty are limited scar lesions, dystrophy and keratoconus.
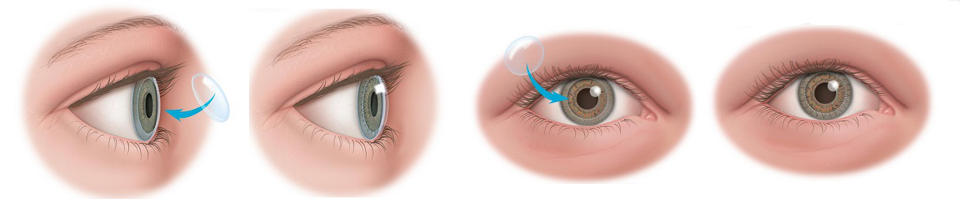
Technique of keratoconus penetrating keratoplasty
1. The size of the graft is determined before the operation using a slit lamp and during the operation by applying trepans of different diameters. The ideal diameter of the flap is 7.5 mm. with its smaller size, there is a probability of developing subsequently high astigmatism, and in the case of flaps with a diameter of 8.5 mm and more, there is a predisposition to the formation of vascularization, synechiae and hypertension of the eye in the postoperative period.
2. Trepanation of the donor cornea is carried out from a pre-prepared corneoscleral flap, which is placed in a concave Teflon block by the endothelium upwards.
The diameter of the graft should exceed the size of the area of trepanation of the patient's eye by 0.25 mm. This is necessary to ensure tightness, minimize postoperative flattening of the cornea and the likelihood of developing glaucoma.

3. The affected tissue is removed carefully to avoid damage to the iris and lens with a trepan:
a) protection of the lens is made by creating pilocarpine myosis before the operation, and during it-the introduction of viscoelastic;
b) it is possible to cut the cornea of the recipient by manual trepan, automatic or vacuum. When using a vacuum trepan reduced slip, because it is tight to the surface. Rapid decompression of the eye, which creates the risk of loss of the eye membranes and expulsive hemorrhage, can be excluded with incomplete trepanation and the use of a diamond knife for subsequent opening of the anterior chamber;
C) completion of the cut is made with a knife or scissors.
The same procedures for the separation of the patient's own cornea and donor graft can be performed using a femtosecond laser.
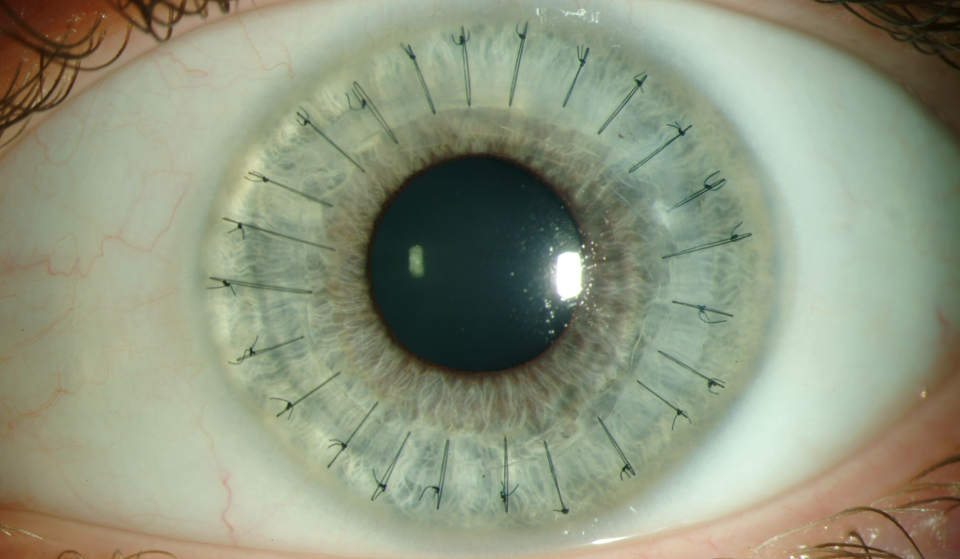
4. Monofilament nylon 10/0 is used to fix donor tissue. The cornea is stitched almost to the full depth so that there is no gaping of the deep edges of the wound, and the descemet's membrane was compared:
a) Firstly, 4 nodal sutures are applied;
b) Secondly, after that imposed any additional interrupted sutures or a continuous circular suture, or a combination thereof.
5. Viscoelastic is replaced by saline (balanced salt solution).
Video of penetrating keratoplasty surgery
Rehab after surgery
1. Local medicinal therapy:
a) Steroids are used to reduce the risk of immune rejection of the implanted graft. Within a few weeks, appoint 4 times a day, and then, depending on the state of the eye, lower the dose. In the future, as a rule, steroids are used in small doses (for example, 1 time per day) for a year or more;
b) Mydriatics are prescribed 2 times a day for two weeks or longer, if there are signs of uveitis.
2. If there is a history of herpesvirus keratitis, Acyclovir (antiviral drugы) is prescribed to prevent its recurrence inside.
3. Suture removal is performed after graft engraftment, usually after 9-12 months. However, in elderly patients, the healing process can take much longer.
4. To improve visual acuity in patients with astigmatism may require hard contact lenses, but they can be used only after complete removal of the sutures.
Possible complications of keratoplasty
- КEarly complications include: delayed epithelialization, external infiltration, irritation from protruding sutures (which can cause capillary hypertrophy), small anterior chamber, uveitis, iris loss, increased intraocular pressure, and infection.
- Late complications: astigmatism, divergence of wound edges, primary pathological process involving graft, occurrence of retrocorneal membrane, cystic edema of the macula and glaucoma.
Transplant rejection reaction
A sign of early insolvency is clouding of the flap from the first day after keratoplasty. The cause may be endothelial dysfunction caused by a defect in the donor's tissue, or an operating trauma.
Late failure results in an immune graft rejection reaction occurring within 6 months after keratoplasty in 50% of all cases or within 1 year.
The process of rejection can affect both the epithelium and endothelium:
a) Characteristic features of epithelial rejection are linear epithelial opacities, which are relatively asymptomatic and have not particularly significant long-term effects. In the future, there are many small subepithelial infiltrates, similar in clinical picture to adenovirus keratitis, which may be accompanied by moderate irit. Intensive local therapy with steroids, as a rule, stops the progression of this process.
b) Endothelial rejection is more serious, as the immune process damages the endothelial cells, so that they can not regenerate. The result may be a permanent swelling of the cornea. The first characteristic features of endothelial rejection are irit and inflammation in the area of corneal-graft contact. After that, there are linear deposits of precipitates, and swelling of the cornea develops. The therapy consists of intensive instillations and parabulbar injections of steroids, in some cases, the systemic use of immunosuppressors is required.
It is worth noting that even with a successful keratoplasty and the absence of complications, many patients need to wear contact lenses, usually hard gas-permeable, for vision correction due to the roughness of the cornea and high astigmatism.
Contact lenses can be prescribed only after the completion of vision stabilization, which usually requires several months after surgery. Although in some cases this period can vary significantly.
Keratoconus keratoplasty price
The cost of surgery in other clinics may consist of two parts: the price of the biotransplant and the surgery itself. We quote the full price for the operation. At the same time, the final figure is affected only by the complexity of the operation - whether the clouded lens will change to an artificial lens (IOL), the iris will be implanted or other concomitant reconstructive interventions will be carried out.
- Penetrating Keratoplasty (PKP, 1 category) - 300 000 rubbles, 4 650 (us-dollars)
- Penetrating Keratoplasty (PKP, 2 category) - 500 000 rubbles, 7 700 (us-dollars)
- Penetrating Keratoplasty (PKP, 2 category) - 600 000 rubbles, 9 300 (us-dollars)
The cost for surgery is specified taking into account the price of the donor's transplant.
If the cost of operations seems to you high, then take into account that we provide the possibility of femtosecond surgery support. Our doctors are leading ophthalmologists in the World in Keratoconus Treatment, who are a specialists with an unprecedented high rate of success of the operations. The desire to save may result in the need for repeated transplants or complete loss of vision.




Tell me please after what time after keratoplasty you can get behind the wheel? Thank you in advance.
It depends on how successful the rehabilitation period will be: whether there will be an inflammatory reaction and what will be able to achieve visual acuity.
On average, a person returns to normal life in a period of one month to six months. However, vision at this stage can be quite low due to astigmatism caused by sutures.
After removal of stitches (on average a year), visual acuity, as a rule, significantly increases. If it is insufficient, refractive errors are usually corrected with glasses.
Thank you in advance.
You will be unworkable after through keratoplasty for a period of one to two months on the state of the eye.
There are no clear recommendations on this topic. Sex after keratoplasty can be equated to physical activity and avoid it at least a week after the operation (in this period, as a rule, it is necessary to wear a protective .
After that, a control examination of the surgeon is necessary, if everything is in order, then you can have sex, but you need to make sure that there are no poses with a tilt of the head, straining, efforts to raise the partner, etc.
More accurate recommendations will be given by the attending physician, based on the assessment of the healing process in dynamics.
If vision is lower, unfortunately, such sharpness is not enough for safe driving.
Second question: can't you drive right after the surgery?
1) Visual Acuity with correction of 1.0 and 0.7 allows you to control the car.
2) Immediately after the penetrating keratoplasty you can not sit behind the wheel, because the operation is carried out under General anesthesia and you will "move away" from it for another day + the operated eye is sealed with a "curtain".
Beer (as well as any alcohol) after keratoplasty is not recommended, because it reduces the effect of drugs prescribed after surgery (antibacterial and other eye drops).
Therefore, while in the postoperative period you carry out instillation, it is better to refrain from drinking alcohol.
In addition, the state of alcohol intoxication increases the risk of traumatization of the operated eye (and in General) - this should be taken into account for patients after corneal transplantation and be especially vigilant.
My eyes open spruce - fir the way it should be?,and if a long look starts to get slimy, so it should be?
Inflammation in the early postoperative period, as a rule, are a normal reaction to decrease after the patient keratoplasty prescribe anti-inflammatory and antibacterial drops and keratophakia. However, it should be understood that gradually they should decrease.
If these complaints were not at first, and they appeared later (a week after the operation) - this is an occasion for immediate treatment to the doctor of the clinic in which you operated.
What will be the best option for a particular patient is decided only by the attending physician, based on his data and the preferred tactics of such patients.
If you contact one of our specialists - he will inspect and give a competent opinion about your situation.
It doesn't make sense to make any recommendations just based on What you've described.
It is not clear how long time is since the corneal transplantion.
In the postoperative period is not recommended physical activity associated with slopes and lifting weights (up to 9-12 months).
Restrictions are removed by the attending physician after the fact that the healing process was good and there are no risks.
"Light" household chores (Ironing, cooking, but it is necessary to exclude the impact of hot air, the use of a vacuum cleaner, etc.) are not contraindicated.
Ps you have here usually are people with poor eyesight and the captcha is not visible,
Unfortunately, patients who have undergone a corneal transplant must comply with some restrictions not only in the early postoperative period, but also in the future: not recommended heavy physical activity (weight lifting) and sports associated with the risk of eye injury (fighting).
It is also better to give up the sauna, because exposure to high temperatures can adversely affect the corneal transplant.
More detailed recommendations will be given to you by the attending physician during control examinations - based on the current state of the transplanted cornea.
Compliance with the regime after the operation of PKP is an integral part for a successful outcome, because it is necessary not only to bury the drops, but also to comply with the protective regime.
Perhaps you should get the opinion of the neurologist/psychiatrist you are seeing about this.
As for the options of keratoplasty - it is determined based on the condition of the eye of a particular patient and, if you are recommended through transplantation, then this is the best treatment option.
Perhaps we are talking about postoperative astigmatism, affecting visual acuity.
For any forecasts and recommendations it is necessary to have both current diagnostic data (refractometry, corneal OCT, topograpy, etc.) and compare them with the dynamics.
First, you need to decide how it would be advisable to carry out a corneal transplant in terms of improving visual functions (whether the retina is preserved).
Secondly, undoubtedly, the presence of silicone is a factor complicating the operation of keratoplasty. It should be understood, which layers are localized turbidity: maybe You need lamellar keratoplasty. This question can be answered only after face-to-face consultation with a specialist.
Sex, as such, is not contraindicated after corneal transplant surgery, physical activity is contraindicated (associated with jumps, straining, etc.).
Thus, if these activities are excluded from the process, then somehow negatively affect the sexual life of the rehabilitation process should not.
Answers to your questions are not possible without face-to-face consultation, as "turbidity" can be caused by different reasons: refractive errors, graft opacity, etc.
I had an operation penetrating keratoplasty 4 months ago, at the moment the vision fell on the operated eye fell to 0.05, it is planned to tighten the seams due to weakening.
Please tell me:
1. What is the approximate rehabilitation period you can expect after tightening the stitches? (How long before you can get to work)
2. Is it possible to drive for long distances (up to 500 km)
3. Is it possible to fly on airplanes and how much after the pull-up?
4. How much time can be spent at the computer, is it possible to sit at the computer all day?
2) Visual activity (including driving) are not recommended immediately after the procedure, as visual discomfort, instability of vision may be present, and the reduction in the purity of blinking movements leads to drying of the cornea.
3) Usually, restrictions on flights of 1-2 weeks (depending on the state of the eye).
4) within 1-2 weeks long work at the computer undesirable. It is necessary to use moisturizing drops and keratophakia in order to avoid drying of the cornea and damage.
Cancellation is made by the attending physician based on the condition of the eyes of a particular patient (including after removal of stitches).
Undoubtedly, the disease increases the risk of complications such as turbidity or melting of the graft (but, this happens in healthy people), however, if there are indications for corneal transplantation and it will restore vision - try, definitely, it is necessary.
The only class of drugs that are undesirable in this case are Immunostimulants, because they can increase the risk of donor transplant rejection.
Tell me please after PKP took 10 months, the stitches were removed 2 months ago.
I have some questions.:
1. Is it possible to walk in the afternoon under the sun, how critical a long stay in the sun and when you can fully day to walk in a t-shirt or sunbathe?
2. Now for me all also remain restrictions on lifting of weight?
3. Whether it is possible to drink alcohol if now passed only on drops against dryness of an eye.(after all, alcohol is still able to increase the pressure?)
4. Any harmful smoke or just cigarette?
Thank you in advance for answers.
As for the "General" - the lifting of weights is not recommended (more than 10 kg.), about alcohol after corneal transplantation - a moderate amount is allowed.
The Council is associated more with the fact that alcohol intoxication increases the risk of trauma in General and for Eyes in particular.
Son in 16 years was diagnosed with keratoconus. After the examination, segment rings were applied. Every six months, came for a visit. Now we are 20 years old, crosslinking is recommended.
Question: why it is impossible to do PKP firstly?
It is not clear why 4 years have passed after the implantation of the segments, and cross - linking has not yet been done-it is usually carried out 1-6 months after the installation of the rings.